Glaucoma of the eye - what is it, symptoms, treatment. Primary open-angle glaucoma.
Glaucoma is a group of diseases characterized often by increased intraocular pressure (IOP), but not always, visual field changes and disc pathology. optic nerve(excavation up to atrophy).
Causes of glaucoma
Risk factors for developing the disease:
- increased IOP (ophthalmohypertension)
- age over 50
- ethnicity (glaucoma is more common in blacks)
- chronic eye diseases (iridocyclitis, chorioretinitis, cataracts)
- history of eye injury
- common diseases(atherosclerosis, hypertension, obesity, diabetes)
- stress
- long-term use of certain drugs (antidepressants, psychotropic substances, antihistamines, etc.)
- heredity (in families where one of the relatives has glaucoma, there is a risk of developing the disease)
Glaucoma is congenital and acquired. The first type is associated with developmental disorders of the eye in the embryonic period of development. Often these are intrauterine infections - rubella, influenza, toxoplasmosis, mumps, or maternal diseases and the influence of damaging factors (severe endocrine pathologies, high temperatures and radiation).
The main types of acquired glaucoma are primary (open-angle, closed-angle, mixed) and secondary (inflammatory, phacogenous, vascular, traumatic, postoperative).
Symptoms of glaucoma
Signs of open-angle glaucoma include ophthalmohypertension (periodic or constant increase in pressure), visual field loss (in this case, a person does not see part of the surrounding objects).
Open angle glaucoma
Open-angle glaucoma is divided into stages (according to the degree of development of clinical signs) and the level of intraocular pressure.
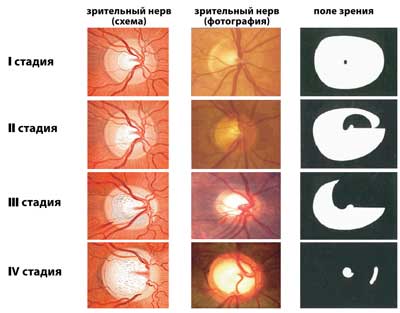
Stages of primary open-angle glaucoma:
Stage I (initial) - there are no changes in peripheral vision, but there are small ones in the central one (paracentral scotomas, in the Bjerrum zone, expansion of the blind spot), excavation of the optic nerve papilla, not reaching its edge.
Stage II (developed) - narrowing of the peripheral field of view more than 10 degrees from the nasal side or concentric narrowing, not reaching 15 degrees from the point of fixation, excavation of the OD (marginal)
Stage III (far advanced) - characterized by a concentric narrowing of the field of view and in one or more segments more than 15 degrees from the fixation point, excavation of the OD
Stage IV (terminal) - complete absence of vision or light perception with incorrect projection, residual vision in the temporal region is possible. If the media of the eye are transparent and the fundus is visible, then there is atrophy of the optic nerve.
According to the level of intraocular pressure, 3 degrees are distinguished:
A-normal IOP (up to 27 mm Hg)
B-moderate IOP (28-32 mmHg)
C-high IOP (more than 33 mmHg)
Separately isolated glaucoma with normal intraocular pressure. At the same time, there are characteristic visual field loss, excavation develops, followed by atrophy of the optic nerve papilla, but IOP is normal.
Angle-closure glaucoma
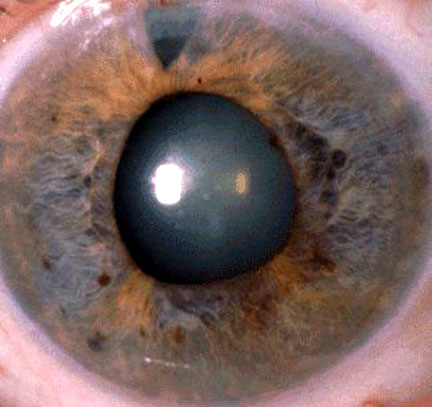
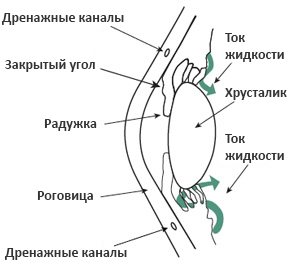
Angle-closure glaucoma occurs in cases of complete or partial blockage of the iridocorneal angle, through which the outflow of aqueous humor occurs. Provoking factors: small eyes (farsightedness often develops), shallow anterior chamber, excessive production of intraocular fluid, large lens, narrow iridocorneal angle (ANC). There is a periodic increase in IOP, the extreme manifestation of which is an acute attack of glaucoma, which can be caused by prolonged exposure to a dark room or at dusk, a large number of drunk liquid, emotional stress. There are severe pains in the eye, radiating to the corresponding half of the head, redness, iridescent circles when looking at the light source.
This condition requires immediate treatment.
Stabilized and non-stabilized glaucoma is also distinguished depending on the degree of progression (by visual acuity and field of view).
Depending on the degree of compensation, glaucoma can be compensated (no negative dynamics), subcompensated (there is a negative dynamics) and decompensated (an acute attack of glaucoma with a sharp deterioration in visual functions).
Glaucoma can be asymptomatic for a long time and patients seek help when some visual functions have already been irretrievably lost.
Symptoms for which you should see a doctor to stop the development of the disease:
- loss of field of view (some objects are not visible)
- rainbow circles when looking at a light source
- blurred vision
- frequent change of glasses
- pain in the brow area
Diagnosis of glaucoma
1. Ophthalmological examination:
- visometry (even with tubular vision, visual acuity can be 100%)
- perimetry, incl. computer. Reveal the slightest changes in the field of view.
- campimetry - examination of the blind spot (the area in the field of view that a person normally does not see) - normally 10 × 12 cm
- biomicroscopy (expansion of the vessels of the conjunctiva, a symptom of the emissary (deposition of pigment along the anterior ciliary vessels), a symptom of the cobra (expansion of the episcleral veins in the form of a funnel before their perforation of the sclera), dystrophy of the iris and pigmented precipitates)
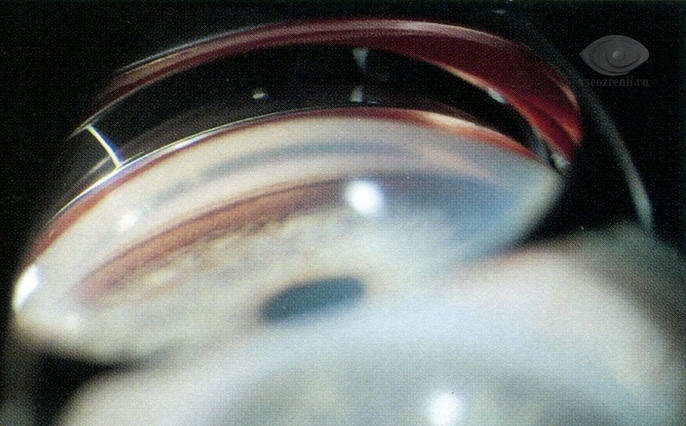
- gonioscopy-examination of the iridocorneal angle using a goniolens (determine the size of the angle of the anterior chamber)
- tonometry according to Maklakov (norm 16-26 mm Hg), non-contact tonometry (not an accurate method, used for mass research)
- tonography - tonometry for 4 minutes using an electronic tonograph. Normal indicators:
P0=10-19 mmHg (true intraocular pressure)
F=1.1-4.0 mm3/min (minute volume of intraocular fluid)
С=0.14-0.56 mm3/min/mm Hg (outflow ease factor)
KB= 30-100 (Becker's ratio= P0/S)
- ophthalmoscopy (determine excavation of the optic disc) and examination with a Goldman lens

- optical coherence tomography of the retina (determine the slightest changes in the optic nerve head)
- Heidelberg retinotomography
- rheoophthalmography (determine the degree of ischemia or hypervolemia of each eye)
- stress tests (help in the diagnosis of angle-closure glaucoma - dark, orthoclinostatic, with mydriatics). In this case, the pupil dilates, the angle of the anterior chamber closes, and symptoms of an acute attack occur.
2. General examination - clinical tests blood and sugar biochemical analysis blood, consultations of a therapist, cardiologist, neuropathologist, endocrinologist to identify concomitant pathology that can provoke the onset or development of complications in patients with glaucoma.
Glaucoma treatment
There is no cure for glaucoma, it can only stop the progression of the disease. Treatment is prescribed only by a doctor.
Types of treatment used for glaucoma:
1. Local drug treatment:
- derivatives of prostaglandins (increase the outflow of intraocular fluid) - Travatan, Xalatan - instill 1 drop in each eye before going to bed
- β-blockers - reduce the production of aqueous humor - (non-selective (do not have side effects on the heart and bronchi, contraindicated in people with bronchospasm) and selective) - Timolol (Arutimol, Kuzimolol 0.25% or 0.5%), Betoptik and Betoptik S. Instill every 12 hours.
- miotics - pilocarpine 1% - used for angle-closure glaucoma (narrow the pupil, the root of the iris moves away from the angle of the anterior chamber, thereby opening it) - 1 drop up to 3 times a day.
- carbonic anhydrase inhibitors reduce the production of intraocular fluid (Azopt, Trusopt) - 1 drop 2 times a day.
First, 1 drug is prescribed (more often these are prostaglandin derivatives). If there is no effect, add other drops, such as β-blockers. Treatment is selected only by a doctor, because. some drugs are toxic and have many contraindications.
Antihypertensive drops are used constantly to slow down the development of glaucoma.
2. Neuroprotectors are required because glaucoma affects the nerve tissue. There are direct and indirect (improve microcirculation and indirectly act on neurons). The direct ones include vitamins C, A, group B, emoxipin, mexidol, histochrome, neuropeptides (retinalamin, cortexin), indirect-theophylline, vinpocetine, pentoxifylline, nootropics, hypocholesterolemic drugs. The patient 1-2 times a year undergoes a course of drug therapy in a hospital.
3. Physiotherapy treatment includes the use of methods such as electrical stimulation of the optic nerve, magnetotherapy, laser therapy.
4. If drug therapy ineffective, surgical treatment (laser or traditional) is indicated.
Glaucoma attack
An acute attack of glaucoma requires immediate treatment. There are arching pains in the eye, radiating to nearby areas, nausea and vomiting, there may be an oculocardial syndrome. On examination, a mixed injection, edematous cornea, anterior chamber is small, dilated pupil, bombardment (bulging) of the iris, the fundus is not clearly visible, the optic nerve with hemorrhages. The eye acquires a stone density.
First of all, the patient is asked when the last time was a chair and urination, blood pressure (BP) is measured. These conditions increase blood pressure. When emptying the intestines, vasospasm is relieved, and there is a high probability that IOP will quickly decrease.
Be sure to often instill pilocarpine 1% and timolol 2 times a day. Intramuscular anesthetics (promedol, analgin). Apply distraction therapy (for example, mustard plasters on the back of the head). They take diacarb with asparkam, intramuscularly lasix under the control of blood pressure. After stopping the attack, surgical treatment is recommended.
Operative treatment of glaucoma
The main types of laser treatment: laser iridectomy(form a hole in the iris) trabeculoplasty(improve the permeability of the trabeculae).
There are many ways of microsurgical treatment. The most widely used method is sinustrabeculectomy, in which a new outflow path of aqueous humor is formed under the conjunctiva, and from there the liquid is absorbed into the surrounding tissues. Other operations are also possible - iridocycloretraction(expand the angle of the anterior chamber), sinusotomy(improved outflow), cyclocoagulation(decreased production of aqueous humor).
Folk remedies are ineffective. Patients are only wasting precious time treating them as the disease progresses.
Complications of glaucoma
Complications with untimely or irrational treatment: blindness, terminal painful glaucoma leads to the removal of the eye.
Prevention of glaucoma
Prevention is the early detection of the disease. In the presence of risk factors, it is necessary to visit an ophthalmologist regularly for examination and measurement of intraocular pressure.
Patients with glaucoma must comply with the regime of work and rest, dosed physical exercise are not contraindicated, bad habits are excluded, you can not drink large amounts of liquid, wear clothes that can impede blood flow in the head area (tight ties, collars).
Ophthalmologist Letyuk T.Z.
Glaucoma is an eye disease with an almost asymptomatic course in which damage to the optic nerve and retina occurs with a characteristic loss of visual fields, usually associated with increased intraocular pressure, leading to blindness if left untreated.
Damage to the optic nerve from glaucoma is irreversible and can eventually lead to blindness. Therefore, it is important to detect glaucoma in time to prevent its progression.
Glaucoma is the second leading cause of blindness in the world, affecting people of all genders, races and ethnicities. More than 1 million patients with glaucoma are currently registered in Russia (Libman E.S., 2009).
Symptoms of glaucoma
Most types of glaucoma, especially on initial stages, is asymptomatic, which is the reason for the late appeal of patients to an ophthalmologist, when the disease reaches an advanced stage, and there are irreversible changes in the optic nerve.
Symptoms that make it possible to suspect glaucoma are: narrowing of the boundaries of the peripheral visual field, visual field defects, sometimes iridescent circles when looking at a light source. Visual acuity can remain quite high.
Thus, glaucoma is an insidious disease with an asymptomatic course at the initial stage. The patient, if he notices a narrowing of the boundaries of the field of view, is already at an advanced stage of the disease. Only an ophthalmologist can suspect and detect glaucoma at the initial stage. Therefore, preventive examinations by an ophthalmologist for people over 40 years of age are mandatory.
An acute attack of glaucoma is characterized by a number of symptoms: sudden blurring or decreased vision, iridescent circles or halos when looking at light sources, pain in the eye that radiates to the temple, sometimes nausea and vomiting. If these symptoms occur, you should immediately go to the nearest eye emergency room to prevent permanent loss of vision.
Types of glaucoma
There are many classifications of glaucoma, but depending on the profile of the angle of the anterior chamber, there are open-angle and closed-angle glaucoma. This is important because open-angle glaucoma flows, as a rule, initially chronically, and angle-closure glaucoma often gives acute attacks of increased pressure, which are extremely destructive for the optic nerve and eye tissues as a whole. There are also low-pressure glaucoma, congenital and secondary glaucoma.
- Primary open-angle glaucoma is the most common form of glaucoma in Russia and is characterized by a chronic course. If left untreated, increased intraocular pressure damages the optic nerve, which is manifested by a gradual narrowing of the boundaries of the visual fields, up to tunnel or blindness. The angle of the anterior chamber is open, and the reason for the increase in intraocular pressure is to increase the resistance of the outflow of fluid through the drainage network. Read more about open-angle glaucoma.
- Primary angle-closure glaucoma is less common in Russia than open-angle glaucoma and is characterized by a special structure of the eye, in which a short anterior-posterior axis and a relatively large lens cause a narrow or closed profile of the anterior chamber angle. (see picture) The disease is almost asymptomatic, patients may experience episodes of blurred vision and unilateral headache in the forehead and temple, the so-called subacute attacks of glaucoma. If you do not start appropriate treatment, then an acute attack of glaucoma can occur with severe irreversible consequences. With this form of glaucoma, intraocular pressure outside the attacks in the initial stages may remain normal. But the special shape of the structure of your eye, namely the angle of the anterior chamber, allows the ophthalmologist to suspect glaucoma or a predisposition to it in time, conduct special examinations for glaucoma and take appropriate preventive or therapeutic measures. Therefore, regular check-ups with an ophthalmologist are extremely important for your vision. Read more about angle-closure glaucoma.
- Low pressure glaucoma or normotension glaucoma or pseudo glaucoma normal pressure- This is a special subspecies of open-angle glaucoma, characterized by a gradual lesion of the optic nerve and corresponding visual field defects, but with normal values of intraocular pressure. It is assumed that the cause of this pathology is inadequate blood supply to the optic nerve, the so-called low perfusion pressure, and extreme sensitivity of the optic nerve even to normal intraocular pressure numbers. Often people suffering from normotensive glaucoma have low blood pressure numbers - hypotension, and may suffer from cervical osteochondrosis.
- Congenital glaucoma is a hereditary form of the disease, which is caused by abnormal development of intraocular structures, which causes fluid retention, increased intraocular pressure, enlargement of the diameter and swelling of the cornea.
congenital glaucoma is detected in a child, usually under the age of one year by a pediatrician or pediatric ophthalmologist and almost always requires surgical treatment. - Secondary glaucoma is usually caused by other eye diseases: eye injuries, long-term inflammatory diseases (uveitis, iridocyclitis), changes in the position of the lens or its volume, intraocular tumors, etc. Long-term use of corticosteroids, for example, by patients with bronchial asthma or systemic autoimmune diseases, can cause the development of secondary steroid glaucoma.
Diagnosis of glaucoma
The person himself does not feel the increased intraocular pressure, it can only be determined with the help of a special study - tonometry. Tonometry can be contact, when a special weight is applied to the eye, and non-contact, using special devices - pneumotonometers.
Damage to the optic nerve in glaucoma is manifested by a narrowing of the boundaries of the visual field, so the study of visual fields or perimetry is a mandatory method of examination for glaucoma. Patients themselves rarely notice a change in their peripheral visual field, especially of an initial nature, which is why ophthalmologists often detect already developed and advanced stages of glaucoma.
During biomicroscopy of the anterior segment of the eye, an ophthalmologist may notice changes characteristic of various types of glaucoma and suspect it. To see the angle of the anterior chamber and evaluate its shape and condition, it is necessary to conduct a study - gonioscopy.
Examination of the fundus or ophthalmoscopy allows you to assess the condition of the optic nerve, retina, blood vessels. Ophthalmoscopy can be performed by contact, when a special lens is attached to the eye, but more often it is performed non-contact with the help of magnifying lenses and / or a special device - an ophthalmoscope.
Currently, ophthalmologists use high-tech examination methods for diagnosing glaucoma, such as Heidelberg retinal tomography and optical coherence tomography. These methods make it possible to determine with high accuracy the thickness of the nerve fiber layer in the area of the optic nerve head, its excavation and other parameters, the assessment of which is extremely important both in the primary diagnosis of glaucoma and in the control of its course.
Ultrasonic biomicroscopy allows to visualize in detail the structure of the eye, including the outflow tracts of intraocular fluid, gives an idea of the size and ratio of intraocular structures that are not available for visualization by ophthalmoscopy methods.
You can read more about methods for diagnosing glaucoma in the Glaucoma Examination section.
Glaucoma treatment
Unfortunately, today there are no methods to cure, cure glaucoma, but it must and can be treated and controlled. Depending on the type, stage and severity of the disease, the ophthalmologist will prescribe drops for glaucoma, recommend laser treatment or suggest surgery.
As a rule, treatment begins with the appointment of eye drops of various types, which have one property - they reduce intraocular pressure and, thereby, prevent damage to the optic nerve. But these drops need to be dripped constantly, on schedule, because. their period of action in the eye is limited. Some drops may cause a feeling of discomfort, burning in the eye, but this is not a reason to cancel the drops on your own without first consulting an ophthalmologist about the possibility of replacing them with others.

Regardless of the treatment, early diagnosis of glaucoma is the best way to avoid blindness. Therefore, preventive examinations by an ophthalmologist are simply necessary for the early detection of glaucoma, especially if you have risk factors for developing this disease.
The asymptomatic and painless course of the disease causes the frivolous attitude of some patients to the prescribed treatment, who drip drops irregularly, or even stop altogether, forget to purchase a new bottle of drops in advance, and do not appear at the appointed time at the control examination by an ophthalmologist. This attitude to treatment is the cause of the progression of glaucoma and, as a result, irreversible loss of vision.
Patient adherence to treatment is one of the main success factors in the fight against glaucoma.
GLAUCOMA It is an eye disease caused by an increase in intraocular pressure. If eye pressure in glaucoma is not reduced to normal in time, the optic nerve may die, which leads to irreversible blindness.
GLAUCOMA - WHAT IS HIGH INTRAOCULAR PRESSURE DANGEROUS IN GLAUCOMA?
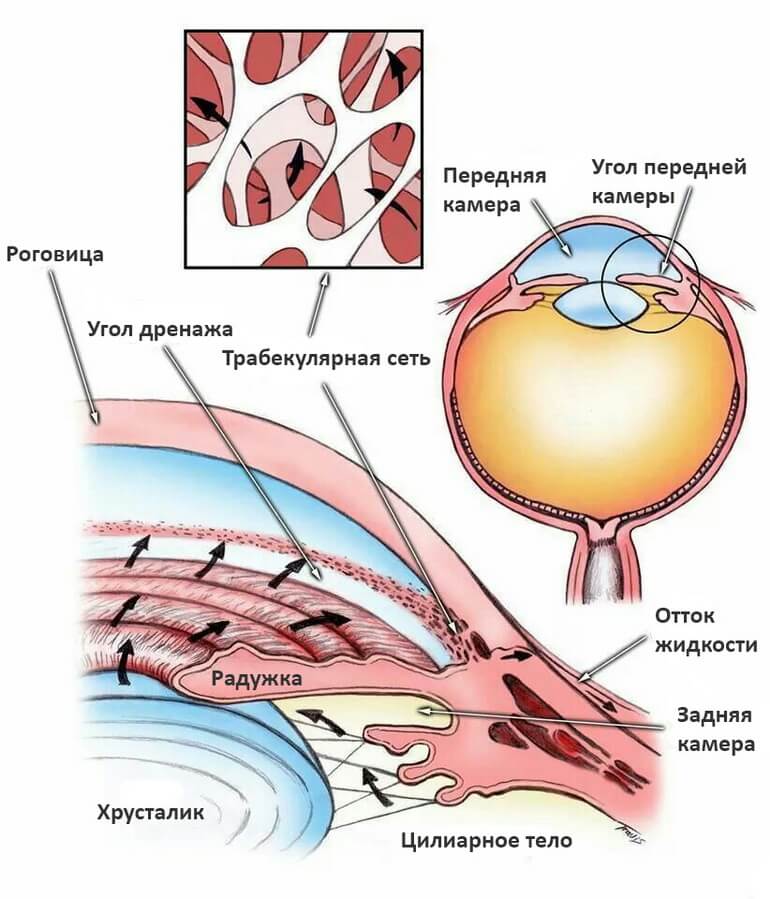
A healthy eye has a constant intraocular pressure (18-22 mm Hg), due to the balance of fluid inflow and outflow. In glaucoma, the circulation of fluid in the eye is disturbed, it accumulates, and intraocular pressure begins to rise. In this case, the optic nerve and other structures of the eye experience an increased load, the blood supply to the eye suffers.
As a result, glaucoma affects the visual function of the eye. At the beginning, a person simply begins to see worse, then peripheral vision is disturbed, the visibility zone is limited, and eventually blindness may occur. Moreover, these changes are irreversible, which is why it is so important to start glaucoma treatment on time. Glaucoma also causes sudden loss of vision.
GLAUCOMA - WHAT YOU NEED TO KNOW ABOUT GLAUCOMA
Glaucoma is insidious - it creeps up imperceptibly, can carry out hidden destructive work for a long time, in order to then burst into a sudden, seemingly catastrophe. Untreated, advanced glaucoma inevitably leads to reduced vision and complete blindness. The eye, no longer distinguishing light, can cause severe pain, and then there is nothing left but to remove it. Keeping this in mind, you probably will not be too lazy to visit an ophthalmologist's office and check the condition of your eyes.
Young people get glaucoma rarely, it usually develops after 40 years. If you are at this age, a preventive examination is a must. Diabetes mellitus and atherosclerosis predispose to the development of glaucoma. People suffering from these diseases should pay special attention to protecting their eyesight. Hereditary predisposition to glaucoma has been established. If any of your blood relatives have had or are suffering from glaucoma, you are at increased risk.
The essence of this disease is a periodic or constant increase in intraocular pressure. Why is it rising? Imagine the events that take place day and night in your eye: every minute about two cubic millimeters of moisture enters it and the same amount must flow out. The value of intraocular pressure is determined by the balance of inflow and outflow, and in glaucoma the outflow is disturbed, excess moisture remains in the eye, and the pressure rises. The fact is that moisture flows through a special drainage system, consisting of a porous diaphragm, which is located in the corner of the anterior chamber of the eye, and microscopic tubules that remove moisture after filtration through the diaphragm into small blood vessels on the surface of the eye. Increased pressure compresses, deforms the outflow of fluid, which contributes to a further rise in IOP.
You may not feel high blood pressure but that doesn't make it any less dangerous. The higher the pressure, the longer it remains at high levels, the more the optic nerve suffers. Gradually, its atrophy sets in, it fades, dies. And with it, vision dies. Normal intraocular pressure is considered to be between 9 and 22 mm. rt. Art. But if your blood pressure was measured with a Maklakov tonometer and it turned out to be a little higher - do not be alarmed! At the time of measurement, the tonometer (weight) presses on the eye, which increases the performance. The so-called tonometric pressure is considered normal within 17-26 mm. rt. Art.
Having established glaucoma, the doctor usually tells you its form - open-angle or closed-angle. The difference between them is in the mechanism that increases the pressure. Angle-closure glaucoma occurs when the peripheral iris blocks the angle of the anterior chamber of the eye, making it difficult for fluid to reach the drainage system. Having no way out, it accumulates in the eye, and intraocular pressure rises. With an open-angled form, access to the drainage system is open, but its own filtration capacity is impaired, and therefore moisture again flows out of the eye with difficulty. The end result is the same - an increase in intraocular pressure.
The open-angle form is “worse”, perhaps, only because it is asymptomatic for a particularly long time and is detected already in the later stages. Angle-closure is more frank - with a strong increase in pressure, it can declare itself with an acute attack: pain occurs in the eye, superciliary arch, temple, the affected eye seems to be covered with fog, when looking at a lamp or other light source, iridescent circles appear.
The attack can be stronger and weaker, more often it occurs in the evening. So, you need to hurry to the doctor immediately! A mixed form of glaucoma is also possible, when there is both a partial blockade of the angle of the anterior chamber of the eye, and a deterioration in the filtration capacity of the drainage system.
In the conclusion that the doctor will write to you, there may be Latin letters A, B, C. This is how the level of intraocular pressure is indicated: A - within normal limits, B - moderately elevated (up to 33 mm Hg), C - high (above 33 mmHg.). The following diagnosis is also possible: “Normal pressure glaucoma”. Most often in these cases, the pressure is kept in the zone of the upper limit of the norm, but the blood circulation in the optic nerve is sharply worsened and, therefore, its functions are impaired. The doctor selects the treatment taking into account not only the characteristics of glaucoma, but also your general condition.
It is almost impossible to completely cure this disease - it is chronic. But with timely started correct and systematic treatment, the development of glaucoma can be stopped and saved. good vision. Tune in to resist the disease, which means accurate, accurate, patient fulfillment of doctor's prescriptions. The basis of treatment is drugs that reduce intraocular pressure. As a rule, these are eye drops, and it is likely that you will have to bury them all your life. However, you have a chance: with age, glaucoma can become "burnt out" - this means that vision is maintained within certain limits, pressure stabilizes, so there is no longer a need to constantly lower it.
The instillation technique is simple, you can easily master it yourself, and very soon this procedure will become as familiar as, say, brushing your teeth in the mornings and evenings. So, look up, pull the lower eyelid with the index finger of one hand, and instill the medicine with the other. The conjunctiva holds only one drop, no more is required. Bury the second one if you are not sure of the exact hit. Try not to touch the eyelashes and the eyeball with the tip of the pipette, so as not to violate the sterility of the medicine and not to injure the eye. True, most vials of eye drops are now equipped with plastic droppers with a safety tip. If you are prescribed pilocarpine, pay attention - in which version. Water solution need to be instilled 3-4 times a day, and solutions prolonged action(on methylcellulose, polyvinyl alcohol) - only 2-3 times a day.
Timolol maleate is now widely used to treat all types of glaucoma. In pharmacies, this drug comes under different names: oftan timolol, okumed, timoptik. Timolol is not only effective, but also convenient - it is usually instilled only 1-2 times a day. Best before date eye drops factory production - at least 2 years, but after opening the bottle they can be used for no more than a month. Prepared in a pharmacy have a short shelf life - 7 days from the date of preparation. These and other drops can be stored before opening the bottle at room temperature in a dark place, and after opening - in the refrigerator. Like any medicine, eye drops can have and side effect. For example, clonidine (clonidine), by reducing intraocular pressure, can simultaneously reduce the total arterial pressure, which, for example, is undesirable for a hypotensive patient.
Hypersensitivity to a particular drug is possible, and then immediately after instillation there is a burning sensation, discomfort, the eye may turn red, and sometimes it begins headache, heartbeat quickens, arrhythmia appears. Such sensations must be reported to the doctor, and he will select another remedy or advise how to mitigate the complications that arise. For an ophthalmologist, information is also important about what chronic diseases you suffer from. After all, some eye drops are contraindicated in diabetes, bronchial asthma, chronic diseases lungs, heart failure. Such patients are usually prescribed betaxolol (betoptik).
In the treatment of glaucoma, not only eye drops are used, but also drugs taken orally, for example, acetazolamide (diacarb). This drug, which reduces the production of intraocular fluid, also has a moderate diuretic effect, and potassium, which is necessary for cardiac activity, is washed out with urine. Therefore, together with diacarb, potassium orotate, panangin are usually prescribed. Try to enrich your diet with foods that contain a lot of potassium. These are baked potatoes, dried apricots, zucchini, bananas. Glycerol is also taken inside in the form of a 50% solution. It can be diluted to improve taste. fruit juice, add citric acid. This drug is usually prescribed for an acute attack of glaucoma. If you have such an attack, and it is impossible to get to the doctor quickly and there is no glycerol on hand either, use a saline laxative, for example, magnesium sulfate ("bitter salt"), dissolving about 30 g (full tablespoon) in 1 / ^ glass of water . To the complex drug treatment glaucoma also includes agents that improve cerebral circulation, stimulate metabolic processes - trental, vinpocetine, cavinton, multivitamins. Perhaps you are taking such drugs as prescribed by a therapist or neurologist - tell your eye doctor about this so that he can correct the treatment.
If you are offered physiotherapy, in particular, stimulation of the optic nerve and retina using weak electric currents or magnetic fields, feel free to go for these procedures! They are quite effective and completely safe. Treat with confidence and surgical methods- an operation can be a lifesaver for you in a situation where other means have already been exhausted. Surgical interventions for glaucoma are now well developed, performed quickly and painlessly. Do not delay the operation - time is precious in the treatment of glaucoma! The course of this disease largely depends on your lifestyle.
- Work as much as age and general health allow, do not strain. Avoid physical and nervous overload. The maximum weight that can be lifted is 10 kg.
- Even weeding the beds can become overload for you if you work on an incline. Adapt some bench, chair - and do not bend over. Whatever you do - read, draw, knit, do not sit with your head tilted and in poor lighting.
- You can watch TV, but also in good lighting (not in the dark!) And in the right position so that your head is neither tilted nor thrown back.
- When reading and other intense visual work, take small breaks every hour, for 10-15 minutes.
- Eat rationally according to age, prefer vegetable dishes, fish, raw vegetables and fruits, limit animal fats and sugar.
- Liquid, if there are no other indications for this, can not be particularly limited, but you can not immediately drink more than a glass. Tea is even useful, since the caffeine contained in it improves blood circulation in the tissues of the eyes, and increases intraocular pressure in rare cases. A cup of coffee is also not forbidden, but to be sure, it is better to do a caffeine test: measure intraocular pressure before you drink coffee, and 1-1.5 hours after that.
- If you are a smoker - stop smoking immediately! Nicotine is bad for your eyes.
- Do not wear tight collars, ties - anything that impedes blood circulation in the head and neck.
- Good sleep is very important to you. Enter evening walks into the daily routine; if you can’t sleep, take 2-3 teaspoons of honey at night with warm water, do warm foot baths.
- Accurately observe the prescribed mode of instillation of drops. If you have to leave home for a long time, be sure to take them with you.
- With closed-angle glaucoma, a sharp change in lighting is difficult for the eyes. Take pilocarpine before going to the cinema or other darkened rooms to prevent pupil dilation.
- Visit your doctor regularly. Even when intraocular pressure stabilizes, a follow-up examination is recommended every 3 months.
A. P. NESTEROV Professor, Academician of RAMS and RAMTS
E. A. EGOROV Professor, Academician of RAMTS
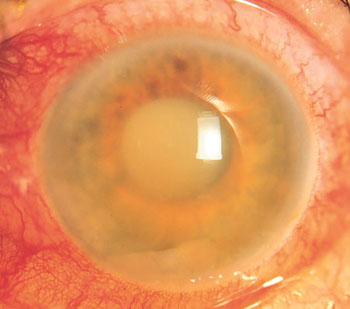
Glaucoma is a group of eye diseases that lead to damage to the optic nerve and loss of vision. The most common form is open-angle glaucoma. Less common forms of this disease include angle-closure glaucoma and normal-tension glaucoma (NTG). Open-angle glaucoma develops slowly over a long period of time and does not cause pain. Peripheral vision may begin to deteriorate, followed by deterioration in central vision, resulting in blindness if left untreated. Angle-closure glaucoma may appear gradually or suddenly. The sudden onset may be accompanied by severe eye pain, blurred vision, dilated pupils, red eyes, and nausea. Loss of vision from glaucoma once it occurs is irreversible.
Risk factors for glaucoma include increased intraocular pressure, family history of the disease (heredity), migraine, high blood pressure, and obesity. Intraocular pressure more than 21 mm Hg. (2.8 kPa) or higher increases the risk of developing glaucoma. However, some people may have high eye pressure for years and never develop damage. Conversely, damage to the optic nerve can occur with normal pressure, a condition known as normal pressure glaucoma. The mechanism of development of open-angle glaucoma is believed to be the slow release of aqueous humor through the trabecular meshwork, while in angle-closure glaucoma the iris blocks the trabecular meshwork. Diagnosis is based on an extended eye examination.
At early treatment it is possible to slow or stop the progression of the disease with medication, laser treatment, or surgery. The purpose of these procedures is to reduce intraocular pressure. There are a number of different classes of drugs for the treatment of glaucoma. Laser therapy can be effective in both open-angle and closed-angle glaucoma. A number of types of glaucoma surgery can be used in people who do not respond well to other treatments. Angle-closure glaucoma should be treated as soon as possible.
Between 11 and 67 million people suffer from glaucoma worldwide. This disease is more common in older people. Angle-closure glaucoma is more common in women. Glaucoma is often referred to as the "silent thief of vision" because vision loss usually occurs slowly over a long period of time. Worldwide, glaucoma is the second leading cause of blindness after cataracts. The word "glaucoma" comes from the ancient Greek word " glaukos”, which means blue, green or gray. AT English language the word was in use as early as 1587, but did not come into common use until 1850, when the development of the ophthalmoscope allowed people to see damage to the optic nerve.
Forms of glaucoma
There are several forms of glaucoma. The two main forms are:
- open-angle glaucoma
- angle-closure glaucoma
They are characterized by an increase in intraocular pressure (IOP).
This is the most common form of glaucoma, accounting for at least 90% of all cases of this disease:
- It is caused by slow clogging of the drainage channels, which leads to increased intraocular pressure.
- It has a wide and open angle between the iris and cornea.
- It develops slowly and is a lifelong disease.
- Has symptoms and damage that often go unnoticed.
"Open" means that the angle where the iris meets the cornea is as wide and open as it should be. Open-angle glaucoma is also called primary or chronic glaucoma.
This is a less common form of glaucoma:
- It is caused by blockage of the drainage channels, which leads to a sharp increase in intraocular pressure.
- Has a closed or narrow angle between the iris and cornea.
- It develops very quickly.
- Usually causes very noticeable symptoms and damage.
- Requires immediate medical attention.
Normotension glaucoma (NTG)
This form is also called low pressure glaucoma or normal pressure glaucoma. In normotensive glaucoma, the optic nerve is damaged even if the eye pressure is not very high. We still don't know why some people's optic nerves get damaged, even if they have near-normal levels of intraocular pressure.
congenital glaucoma
This form of glaucoma occurs in infants when abnormal or incomplete development of the eye's drainage channels occurs during the prenatal period. This is a rare disease that can be inherited. In the absence of complications, microsurgery can often correct structural defects. Other cases are treated with medications and surgery.
Secondary glaucoma
Secondary glaucoma refers to any condition where another disease causes or contributes to an increase in intraocular pressure, resulting in damage to the optic nerve and loss of vision.
Secondary glaucoma may result from trauma to the eye, inflammation, tumor, or in advanced cases of cataracts or diabetes mellitus. This type of glaucoma can also be caused by certain medications such as steroids. It can be mild or severe. The type of treatment will depend on whether it is open-angle or angle-closure glaucoma.
Pigmentary glaucoma
Pigmentary glaucoma is a form of secondary open-angle glaucoma. It occurs when pigment granules that are found in the back of the iris (the colored part of the eye) penetrate the clear fluid that forms inside the eye. These tiny granules of pigment flow to the drainage channels in the eye and slowly clog them, causing an increase in intraocular pressure. Treatment usually includes drug treatment, laser surgery or conventional surgery.
Pseudoexfoliative glaucoma
This form of secondary open-angle glaucoma occurs when a flaky, dandruff-like material peels off from the outer layer of the lens inside the eye. Material collects in the angle between the cornea and iris and can clog drainage system eyes, causing an increase in intraocular pressure. Pseudoexfoliative glaucoma is common in people of Scandinavian origin. Treatment usually involves medication or surgery.
Traumatic glaucoma
Trauma to the eye can cause secondary open-angle glaucoma. Traumatic glaucoma can occur immediately after an injury or years later. This disease can be caused by blunt or penetrating trauma to the eye. In addition, conditions such as severe myopia, previous trauma, infection, or previous surgery can make the eye more vulnerable to serious eye injury.
Neovascular glaucoma
abnormal formation of new blood vessels on the iris and in the drainage channels of the eye can cause the development of secondary open-angle glaucoma.
Neovascular glaucoma is always associated with other anomalies, and most often with diabetes mellitus. This form of glaucoma never occurs on its own. The new blood vessels block the flow of fluid in the eye through the trabecular meshwork (the drainage channels of the eye), causing an increase in intraocular pressure. This type of glaucoma is very difficult to treat.
Iridocorneal endothelial syndrome (IES)
This rare form of glaucoma usually only appears in one eye, not both. Cells on the posterior surface of the cornea spread along the drainage tissue of the eye and over the surface of the iris, increasing intraocular pressure and damaging the optic nerve. These corneal cells also form adhesions that connect the iris to the cornea, further blocking drainage.
Causes of glaucoma
Glaucoma is usually caused by an inability to maintain a proper balance between the amount of internal (intraocular) fluid produced and the amount of fluid drained into the eye.
The underlying causes of this imbalance are usually related to the form of glaucoma that the person suffers from.
The eyeball needs internal fluid pressure to maintain its globe-like shape and ability to see. But when something interferes with the ability of internal eye structures to regulate intraocular pressure, eye pressure can rise to dangerously high levels, causing glaucoma.
In glaucoma, the eye cannot relieve pressure by draining excess fluid when the pressure is too high. Instead, high eye pressure simply continues to build up and press on the optic nerve until the nerve fibers are irreversibly damaged and vision is lost.
Glaucoma and ocular anatomy
As glaucoma progresses, neuronal damage eventually leads to eye damage in the form of loss of peripheral vision. However, damage to the eyes seems to start first in the brain as the connection is lost.
This discovery, reported in early 2010, is a major breakthrough with the potential to improve early diagnosis and treatment of eye disease, according to researchers Vander Institute of Eye (VEI) in Nashville USA.
To understand what causes glaucoma, you first need to know a few things about anatomy. human eye and about how aqueous humor moves through the eye:
- The clear fluid inside the eye is created by the ciliary body, which is a small, round structure located behind the iris, or the colored part of the eye.
- This fluid, known as aqueous humor, flows behind the iris and through the pupil, or central opening in the middle of the iris. The aqueous humor then fills the anterior chamber, the gap between the back of the transparent cornea and the front of the iris.
- Moisture is expelled from the eye through a structure known as the drainage angle, which is the angle formed within the anterior chamber between the iris and the peripheral cornea.
- Moisture seeps through this corner and through the sclera, or white part of the eye, and then connects to a network of veins outside the eye.
- Any disruption of this outflow of aqueous humor, including in connection with some eye injuries, can lead to an increase in intraocular pressure.
Anatomically, the drainage angle of the eye is called "open" or "closed" (narrow). The narrower the angle, the more difficult it is for aqueous humor to flow through it. An open angle can also impede the outflow of moisture if structural damage is present inside the eye tissues of the angle itself.
Other causes of glaucoma: poor blood flow, damage to the optic nerve
Although high intraocular pressure (URH) is often associated with glaucoma, this eye disease can also occur when there is normal internal eye pressure (normotension glaucoma). People with this condition have highly pressure-sensitive optic nerves that are susceptible to permanent damage from what is generally considered "normal" IOP. Conversely, some people with increased intraocular pressure, known as ocular hypertension, may never develop glaucoma.
Most traditional screening methods for glaucoma involve testing the eyes for high IOP. But because glaucoma can occur even without high IOP, direct examination of the optic nerve and visual field testing are essential in establishing (or ruling out) a diagnosis of glaucoma.
Although the exact cause of normotension glaucoma is unknown, many researchers believe that reduced blood supply to the optic nerve may be a risk factor. This can be caused by constriction of the blood vessels that feed the optic nerve or narrowing of these vessels (vasospasm).
Some studies also show that poor blood flow in the eye is associated with blind spots (scotomas) that develop within the visual field, similar to those that occur with glaucoma.
An intriguing study published in August 2007 points to a potential common cause of both glaucoma and Alzheimer's disease, which creates brain damage and memory loss.
Researchers from the UK have found that the accumulation of beta-amyloid proteins in the retina and brain tissue appears to be associated with the development of both glaucoma and Alzheimer's disease.
However, an abnormal accumulation of beta-amyloid proteins does not mean that a person with Alzheimer's disease will have glaucoma, or vice versa. The researchers say similarities between some eye and brain tissues may explain why the accumulation of beta-amyloid proteins can affect both the eye and the brain.
Symptoms of glaucoma
Glaucoma is a complex disease in which damage to the optic nerve leads to vision loss. As you saw above, there are several forms of glaucoma. The two most common forms are:
- primary open-angle glaucoma (POAG)
- primary angle-closure glaucoma (PACG)
Open-angle glaucoma is often referred to as the "silent thief of vision" because it has no symptoms until significant vision loss has occurred.
Symptoms of Open Angle Glaucoma
Signs or symptoms of open-angle glaucoma are usually absent in the early stages. This disease develops slowly and sometimes without noticeable loss of vision over many years.
Most people with open-angle glaucoma do well and do not notice changes in their vision because the initial loss of vision affects lateral or peripheral vision, and visual acuity is maintained until the disease is advanced.
By the time the patient becomes aware of the loss of vision, the disease is usually quite advanced. Vision loss in glaucoma is irreversible, even with surgery. Because open-angle glaucoma has few warning signs or symptoms before damage has occurred, it's important to see a doctor for regular eye exams. If an eye exam reveals glaucoma, the ophthalmologist may prescribe preventive treatment to protect your vision.
In open-angle glaucoma, the angle in the eye where the iris meets the cornea is as wide and open as it should be, but the eye's drainage channels become clogged over time, causing an increase in internal eye pressure and subsequent damage to the optic nerve. This is the most common type of glaucoma, occurring in 90% of cases in people, many of whom are unaware of the presence of the disease.
The risk of developing glaucoma is increased if your parents or siblings have the disease, and possibly if you have diabetes or cardiovascular disease. The risk of developing glaucoma also increases with age.
Symptoms of angle-closure glaucoma
- blurry or blurred vision
- the appearance of rainbow circles around bright lights
- severe pain in the eyes and head
- nausea or vomiting (accompanying severe eye pain)
- sudden loss of vision
In angle-closure glaucoma, the angle closes in most areas, causing an increase in pressure in the eye, resulting in damage to the optic nerve and possible loss of vision. This increase in intraocular pressure can occur suddenly (an acute attack of angle-closure glaucoma) or gradually. There are also early stages of the disease in which the angle closes but eye pressure may or may not be high and the optic nerve is not yet affected.
The symptoms of acute angle-closure glaucoma are very noticeable and damage occurs quickly. If you experience any of these symptoms, contact your ophthalmologist immediately.
If you've been diagnosed with glaucoma, it's important to set up a regular checkup schedule with your eye doctor to monitor your condition and make sure your prescribed treatment is effectively maintaining a safe eye pressure.
Glaucoma treatment
Glaucoma can be treated with eye drops, medications, laser surgery, conventional surgery, or a combination of these methods. The goal of any treatment is to prevent vision loss, as vision loss in glaucoma is irreversible. The good news is that glaucoma can be controlled if it is detected on early stage, and that with medication and / or surgical treatment most people with glaucoma will not lose their sight.
Taking prescribed medications regularly is critical to preventing vision-threatening damage. That is why it is important for you to discuss side effects with your doctor. Although each drug has some potential side effects, it is important to note that many patients experience no side effects at all. You and your doctor must work as a team in the fight against glaucoma. Your doctor has many options. These include:
Eye drops

If you want to control your eye pressure, it is important to take your medicines regularly and exactly as prescribed. Since the eye drops are absorbed into the blood, tell your doctor about all the medicines you are taking. Ask your doctor and/or pharmacist if it is safe to take your medicines with your prescription glaucoma eye drops. Some drugs can be dangerous when mixed with other drugs. To minimize absorption into the bloodstream and increase the amount of drug absorbed into the eye, close your eyes for one to two minutes after administering the drops and lightly press your index finger against the lower nasal corner of your eyelid to close the tear duct that leads into the nasal cavity. While almost all eye drops may cause an uncomfortable burning or stinging sensation initially, the discomfort should only last a few seconds.
The following types of eye drops are used for glaucoma:
- Eye drops to improve the outflow of intraocular fluid - cholinomimetics. Promote the natural outflow of fluid and effectively reduce IOP. For treatment, a solution of Hydrochloric acid and Pilocarpine are used. Eye drops based on cholinomimetic drugs such as Carbacholin and Aceclidine can only be used as prescribed by a doctor, since they cause a number of side effects. To this group medicines include new drugs such as Travoprost and Latanoprost. These eye drops effectively increase the outflow of aqueous humor through the accessory eye canals.
- Drops to reduce the production of intraocular fluid. This group of drugs includes antihypertensive eye drops - a solution of Betaxolol, Proxodolol, Dorzolamide hydrochloride, Timolol maleate, etc. One of the most used drugs is Timolol maleate, which is used to treat all forms of glaucoma. Preparations based on the active substance Timolol are produced under the name: Arutimol, Oftan timolol, Okumed.
- Combined eye drops. To effectively reduce IOP, drugs with several active ingredients, which not only normalize intraocular pressure, but also reduce the production of aqueous humor. Such combined drugs include: Pilocarpine, Proxodolol, Latanoprost, Fotil, etc.
Tablets
In cases where eye drops do not sufficiently control IOP, in addition to them, medications in the form of tablets. These tablets cause more systemic side effects than eye drops. Their action is also aimed at improving the outflow of intraocular fluid and reducing its production. These drugs are usually taken two to four times a day. It is important to share information about your medications with all your other doctors so that they can prescribe you medications that will not cause potentially harmful interactions.
Your doctor may prescribe one of the following drugs for you:
- Prozerin
- Clonidine
- Cavinton
- Hypothiazide
Surgical procedures (surgery)
When medications do not help or the person experiences unbearable side effects, an ophthalmologist may suggest surgery.
Laser surgery (trabeculoplasty)
This type of surgery is becoming increasingly popular as an intermediate step between medical and conventional surgery, although long-term success rates vary. The most common type performed for open-angle glaucoma is called trabeculoplasty. This procedure takes 10 to 15 minutes, is painless, and can be performed either in a doctor's office or in an outpatient clinic. The laser beam (high energy beam of light) is focused on the trabecular meshwork of the eye. Contrary to what many people think, the laser does not cut a hole in the eye. Instead, the drainage system of the eye is changed in very subtle ways, thereby improving the outflow of intraocular fluid, which leads to a decrease in IOP.
After the operation, you can return home and do your usual daily activities. Your doctor will likely check your IOP one to two hours after laser surgery. After this procedure, many patients experience an improvement in their condition, which makes it possible to avoid or delay surgery. It may take several weeks for the full pressure-lowering effect of this procedure to be felt, during which time you may need to continue taking your medications. Many patients may eventually stop taking some of their prescribed medications. However, you should not stop taking medications on your own. Only your doctor can determine if you still need to take medication or not. Complications from laser surgery are minimal, which is why this procedure is becoming increasingly popular, and some centers recommend trabeculoplasty before using eye drops in selected cases.
Argon laser trabeculoplasty (ALT) - for open-angle glaucoma
The laser processes the trabecular meshwork of the eye, increasing the outflow of intraocular fluid, thereby reducing IOP. In many cases, medication will still be needed. Usually, half of the trabecular meshwork is treated first. If necessary, the other half can be treated as a separate procedure. This method reduces the risk of high blood pressure after surgery. Argon laser trabeculoplasty successfully reduced intraocular pressure in 75% of patients. This type of laser surgery can only be performed two to three times in each eye throughout a lifetime.
Selective laser trabeculoplasty (SLT) - for open-angle glaucoma
SLT is a new laser that uses a very low energy level. It is called "selective" because it leaves sections of the trabecular meshwork intact. For this reason, it is believed that SLT, unlike other types of laser surgery, can be safely repeated. Several authors have reported that rechallenge SLT or SLT after rechallenge ALT is effective in lowering IOP.
Laser peripheral iridotomy (LPI) - for angle-closure glaucoma
This procedure is used to make a hole in the iris of the eye, allowing aqueous humor to flow out of the eye. rear camera through the iris directly into the anterior chamber of the eye. This allows the liquid to pass through normally. ABI is the preferred method for controlling angle-closure glaucoma. This laser is most commonly used to treat anatomically narrow angle and prevent an acute attack of angle-closure glaucoma.
Cycloablation
Two laser treatments for open-angle glaucoma are done to reduce the amount of intraocular fluid by destroying the part of the ciliary body that produces aqueous humor. These procedures are usually performed when conventional treatments have failed, including filtering surgery, or when filtering surgery is not possible or appropriate due to the shape or other features of the eye. Transscleral cyclophotocoagulation uses a laser to direct energy through the outer sclera of the eye to reach and destroy portions of the ciliary processes without causing damage to the overlying tissues. In endoscopic cyclophotocoagulation (CPC), a device is placed inside the eye through a surgical incision so that laser energy is applied directly to the ciliary body tissue.
Traditional surgery
There are the following types of traditional surgical operations with glaucoma:
Trabeculectomy
When medications and laser therapy do not sufficiently reduce intraocular pressure, doctors may recommend conventional surgery. The most common of these surgeries is trabeculectomy, which is used for both open-angle and angle-closure glaucoma. In this procedure, the surgeon creates a passage in the sclera (white part of the eye) to drain excess eye fluid. A valve is created to allow fluid to escape, but not to allow the eye to leak out.
A small bubble of fluid often forms over the opening on the surface of the eye, which is a sign that fluid is draining into the space between the sclera and the conjunctiva. Sometimes the surgically created drainage hole begins to close and the IOP rises again. This is because the body is trying to heal the new hole. Many surgeons perform trabeculectomy with an antifibrotic agent that is placed on the eye during surgery and reduces scarring during the healing period. The most common antifibrotic agent is Mitomycin-C. Another is 5-fluorouracil (5-FU).
About 50% of patients no longer require glaucoma treatment after surgery for a significant period of time. Between 35 and 40% of those who still need treatment have better control of their IOP. Trabeculectomy is usually an outpatient procedure. The number of post-op visits to the doctor varies, and some activities, such as driving, reading, bending over, and weightlifting, should be limited for two to four weeks after surgery.
Drainage system implantation
Several different devices have been developed to facilitate drainage of aqueous humor from the anterior chamber and lower IOP. All of these drainage devices have a similar design, consisting of a small silicone tube that extends into the anterior chamber of the eye. The tube is connected to one or more plates that are sewn to the surface of the eye (usually not visible). The fluid collects on the plate and is then absorbed by the tissues in the eye. This type of surgery is thought to lower IOP less than trabeculectomy, but is preferred in patients whose IOP cannot be controlled with conventional surgery or who have previous scarring.
Non-penetrating surgery
Newer non-penetrating glaucoma surgery, which does not penetrate the anterior chamber of the eye, shows great promise in minimizing postoperative complications and reducing the risk of infection. However, such surgery often requires more skill from the surgeon and usually does not lower IOP in the same way as trabeculectomy. In addition, long-term studies are needed to evaluate these procedures and determine their role in clinical treatment patients with glaucoma.
Some promising surgical alternatives
- Mini Shunt Express- is a stainless steel device that is inserted into the anterior chamber of the eye and placed under the scleral valve. This lowers IOP by diverting intraocular fluid away from the anterior chamber.
- trabektom is a new probe-like device that is inserted into the anterior chamber through the cornea. The procedure uses a small probe that opens the eye's drainage system through a tiny incision and delivers heat energy to the trabecular meshwork, reducing aqueous humor outflow resistance and, as a result, lowering IOP.
- Canaloplasty is the latest advance in non-penetrating surgery designed to improve the circulation of aqueous humor through the trabecular outflow, thereby reducing IOP. Unlike a traditional trabeculectomy, where the surgeon makes a small hole in the eye to allow fluid to drain, canaloplasty is compared to an ocular version of angioplasty, in which the doctor uses an extremely thin catheter to clear the drain.
What is the prognosis for glaucoma
The prognosis depends on when the disease is discovered. If the diagnosis is made before significant damage to the optic nerve, the prognosis is usually good if the patient agrees with the treatment suggested by the ophthalmologist. Since damage to the optic nerve is irreversible and previously damaged optic nerves are more prone to additional damage, delay in diagnosis (when diagnosis is made after significant damage to the optic nerve and partial loss of vision) leads to more aggressive therapy and worsens prognosis.
Can glaucoma be prevented?
Based on our current state of knowledge, primary open-angle glaucoma cannot be prevented. However, optic nerve damage and visual impairment resulting from glaucoma can be prevented by early diagnosis, effective treatment and adherence to the treatment regimen.
Secondary glaucoma can often be prevented by avoiding injury to the eye and by promptly treating eye inflammation and other eye or body conditions that can cause secondary glaucoma.
In most cases, vision loss due to angle-closure glaucoma can be prevented by the appropriate use of laser iridotomy in eyes at risk for developing acute or chronic angle-closure glaucoma.
Marble countertops at great prices thegraniteempire.com.